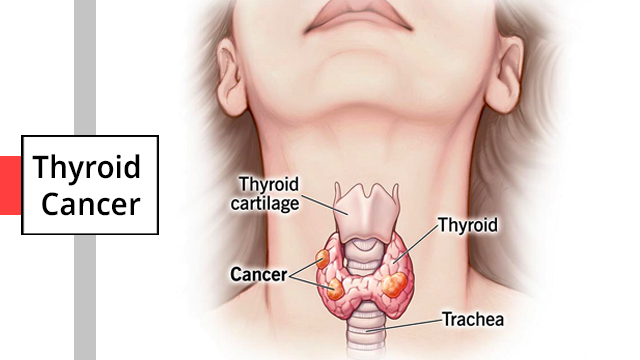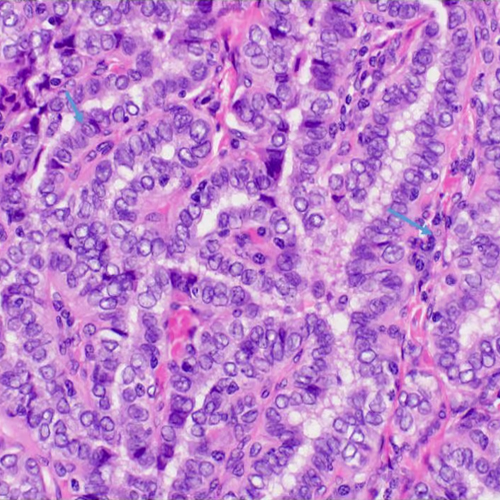
Papillary Thyroid Cancer (PTC)
Papillary thyroid cancer is the most common type, accounting for about 80% of all thyroid cancers. It typically grows slowly and has a good prognosis, with a high likelihood of successful treatment.
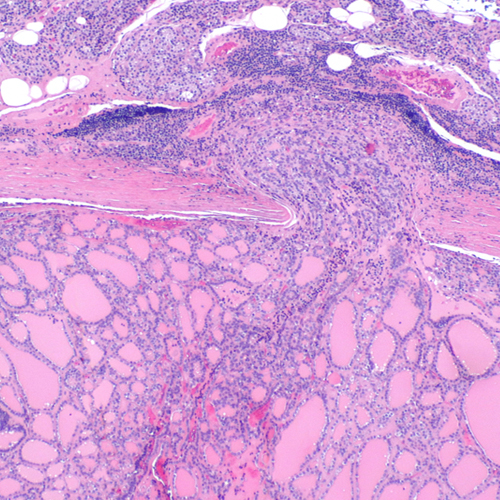
Follicular Thyroid Cancer (FTC)
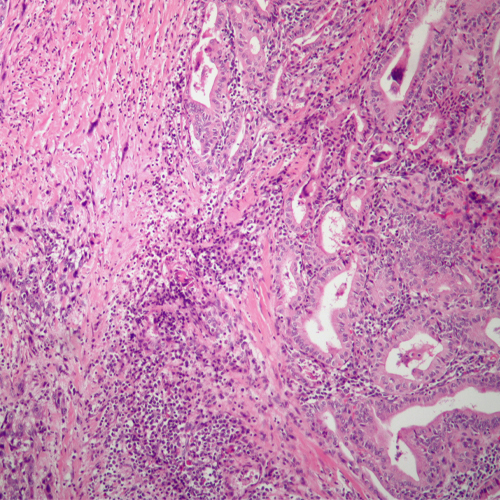
Follicular thyroid cancer is less common than papillary thyroid cancer but still accounts for a significant proportion of cases. It tends to spread to nearby lymph nodes and distant organs more frequently than papillary thyroid cancer.
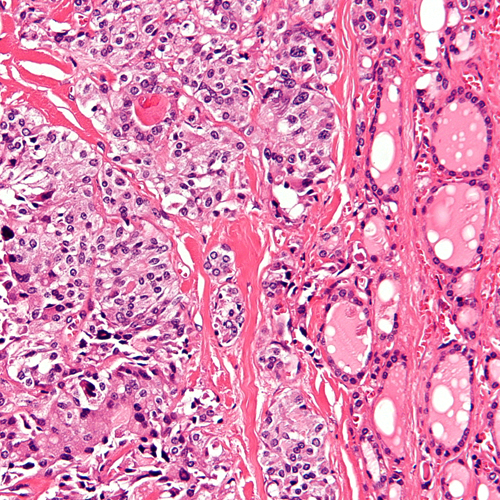
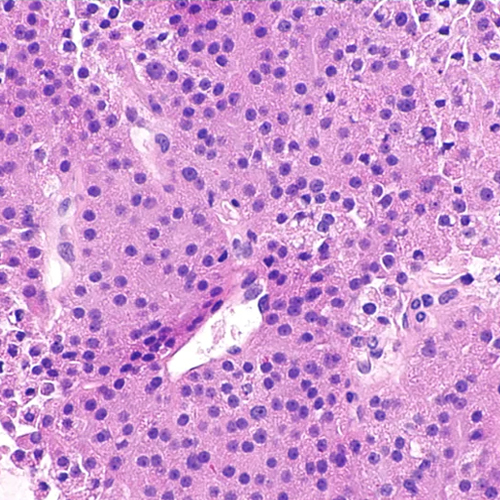
Medullary Thyroid Cancer (MTC)
Medullary thyroid cancer originates from the parafollicular cells of the thyroid gland, which produce calcitonin hormone. MTC can occur sporadically or as a part of a hereditary syndrome called multiple endocrine neoplasia (MEN). It tends to be more aggressive than papillary and follicular thyroid cancers.
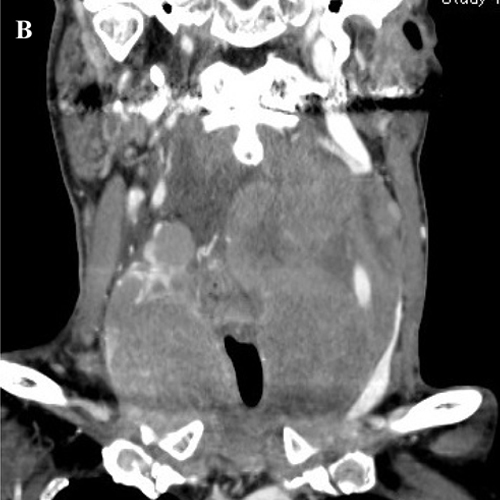
Anaplastic Thyroid Cancer (ATC)
Anaplastic thyroid cancer is rare but highly aggressive. It grows rapidly and is often diagnosed at an advanced stage, making it challenging to treat. Anaplastic thyroid cancer has a poor prognosis compared to other types of thyroid cancer.