Cervical cancer treatment is stage-specific, tailoring interventions based on the extent of the cancer development.
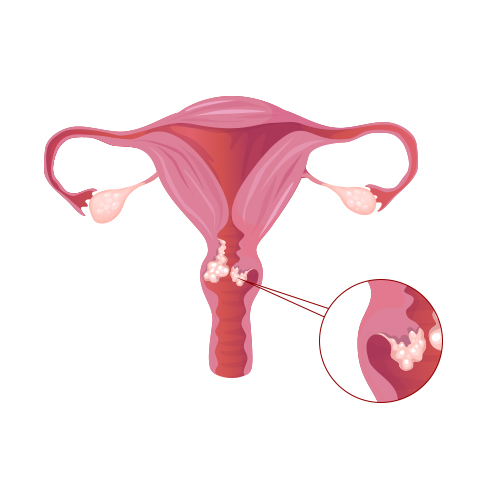
1.Stage 0 (Carcinoma in Situ):
Early-stage cervical cancer, confined to the surface layer of the cervix, often involves surgical removal of abnormal cells through procedures like loop electrosurgical excision procedure (LEEP) or cone biopsy.
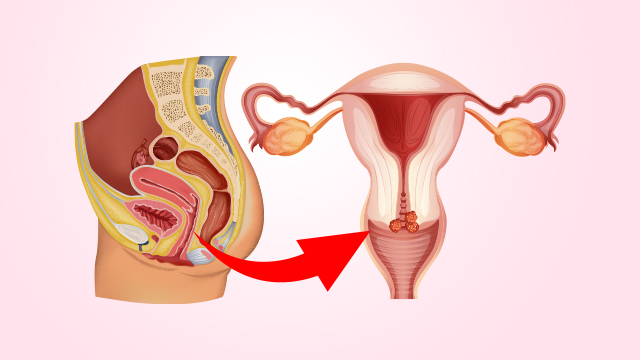
2.Stages I and II:
For localised cancer, surgery remains a primary option, including hysterectomy or removal of lymph nodes. Radiation therapy, either external or internal (brachytherapy), may be employed to target the tumour directly.
3.Stage III:
Cervical cancer that extends beyond the cervix but is confined to the pelvic area may involve a combination of surgery, radiation, and chemotherapy. Radical hysterectomy with removal of surrounding tissues and lymph nodes may be considered.
4.Stage IV:
Advanced-stage cervical cancer, spreading to distant organs, often requires a multidisciplinary approach. Palliative care, chemotherapy, and radiation therapy aim to manage symptoms and improve quality of life.
5.Recurrent Cervical Cancer:
Recurrence may prompt a reassessment of treatment options, including surgery, chemotherapy, targeted therapy, or participation in clinical trials exploring innovative approaches.
Collaboration among oncologists, surgeons, and radiation oncologists ensures a personalised treatment plan. Decisions are based on factors like the patient’s overall health, the tumour’s characteristics, and the potential impact on fertility. Regular follow-ups post-treatment are vital for monitoring recurrence and managing potential side effects. Open communication between healthcare providers and patients is key to navigating the complex landscape of cervical cancer treatment.