Diagnosing blood cancer typically involves a combination of medical history assessment, physical examination, and specialized tests to confirm the presence of abnormal blood cells and determine the specific type and stage of the disease. Common diagnostic procedures include:
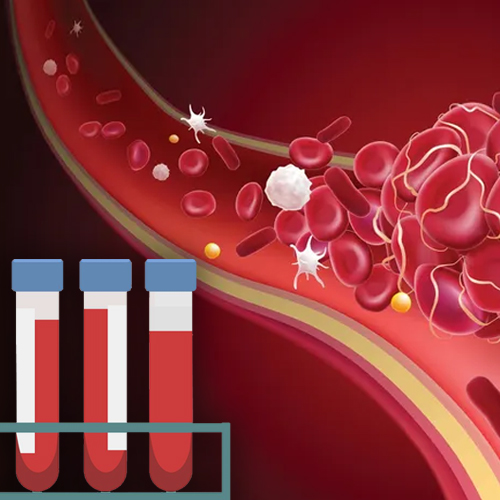
Blood Tests
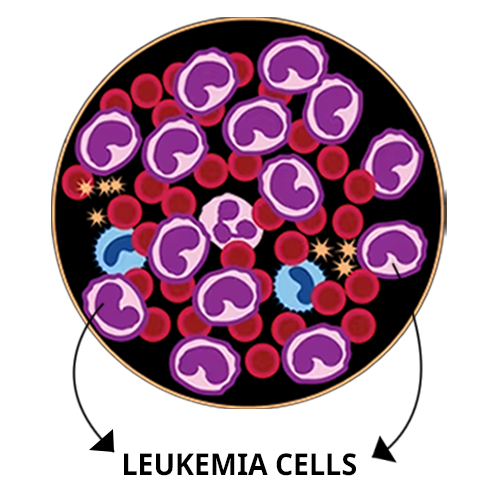
Blood tests, including complete blood count (CBC) and peripheral blood smear, are often the first step in diagnosing blood cancer. These tests can reveal abnormalities in blood cell counts, such as low red blood cell count (anemia), low platelet count (thrombocytopenia), or abnormal white blood cell count.
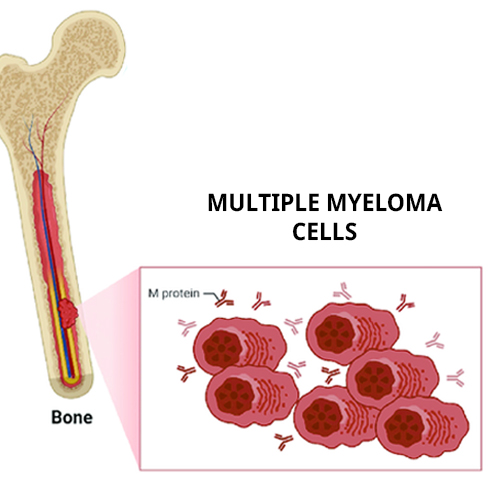
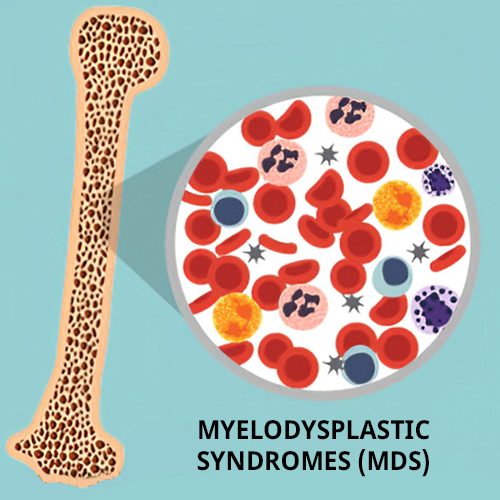
Bone Marrow Aspiration and Biopsy
Bone marrow aspiration and biopsy involve collecting a small sample of bone marrow tissue from the hip bone (pelvic bone) or sternum (breastbone) using a needle. The samples are examined under a microscope to assess the presence of abnormal cells, determine their characteristics, and confirm the blood cancer diagnosis.
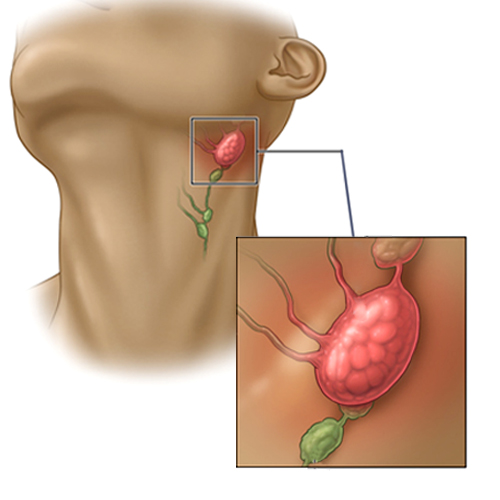
Imaging Studies
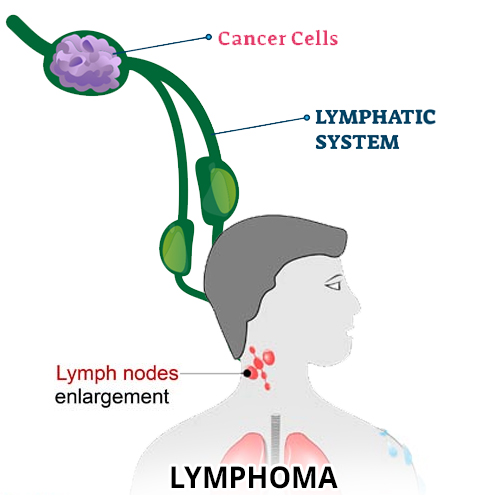
Imaging studies, such as computed tomography (CT) scans, magnetic resonance imaging (MRI), and positron emission tomography (PET) scans, may be used to assess the extent of the disease and identify any abnormalities in the lymph nodes, spleen, or other organs.
Flow Cytometry
Flow cytometry is a laboratory technique used to analyze the characteristics of cells, including their size, shape, and surface proteins. It can help differentiate between normal and abnormal blood cells and classify the type of blood cancer based on specific markers expressed on the cell surface.
Cytogenetic Analysis
The cytogenetic analysis involves examining the chromosomes in blood or bone marrow cells to detect any genetic abnormalities or chromosomal rearrangements associated with blood cancer. This information can help guide treatment decisions and predict prognosis.
Once a diagnosis of blood cancer is confirmed, further tests may be performed to determine the stage of the disease and assess the extent of organ involvement, which helps in developing an appropriate treatment plan.